Sorry, nothing in cart.
Shedding Light on Diabetic Neuropathy
- By admin
- |
- Uncategorized
- |
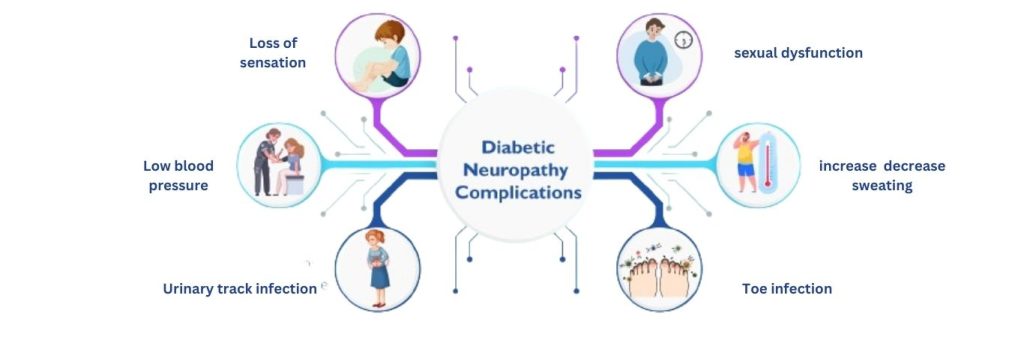
Diabetic neuropathy is a chronic (long-lasting) and common complication of diabetes, affecting millions worldwide. It’s a type of nerve damage that can occur in people who have diabetes. High blood sugar (glucose) in the blood can injure nerves throughout the body. Diabetic neuropathy can affect various nerves. It commonly happens to nerves in the legs and feet.
👉 Consistent blood sugar management and a healthy lifestyle are key factors in preventing or slowing the progression of diabetic neuropathy. By keeping blood sugar levels within a target range, individuals with diabetes can reduce the risk of nerve damage.
👉 Neuropathy can cause pain, and it can vary widely in terms of severity and type of pain experienced. Neuropathic pain is often described as shooting, burning, tingling, or electric shock-like sensations. It can also manifest as a persistent dull ache or throbbing pain.
👉 People suffering from neuropathic pain, obtaining appropriate relief is critical to improve their quality of life. This is when drugs like Aspadol 100mg (tapentadol) come into play.
Type of Neuropathy Pain
There are four main types of diabetic neuropathy. You can have one type or more than one type of neuropathy.

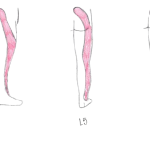
Peripheral Neuropathy: This is the most common type of diabetic neuropathy and affects the nerves that control sensation, typically in the feet, legs, arms, and hands. Symptoms may include numbness, tingling, burning sensations, or pain.
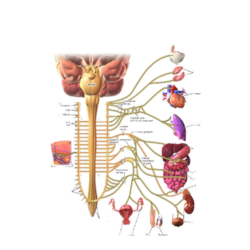
Autonomic Neuropathy: This type affects the nerves that control involuntary bodily functions such as heart rate, digestion, bladder function, and blood pressure. Symptoms may include digestive issues, urinary problems, sexual dysfunction, and difficulty regulating blood pressure.
Proximal Neuropathy (Radiculoplexus Neuropathy, or Diabetic Amyotrophy): This type affects the nerves in the thighs, hips, buttocks, or legs, causing weakness, pain, or numbness. It typically occurs on one side of the body and can lead to difficulty with walking or rising from a seated position.
Focal Neuropathy: Also known as mononeuropathy, this type affects individual nerves, often in the head, torso, or leg. Symptoms depend on the affected nerve and may include sudden onset of pain, weakness, or paralysis in specific areas.
Diabetes can have serious implications for nerve health, leading to diabetic neuropathy and related complications. With proper diabetes management through blood sugar control, lifestyle modifications, regular monitoring, and timely intervention, individuals can reduce the risk and severity of nerve damage and maintain better nerve health and overall quality of life.
Causes of diabetic neuropathy
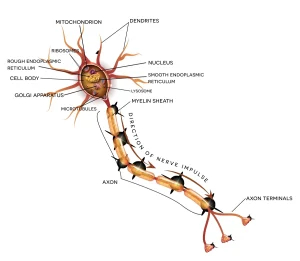
Nerves play a crucial role in transmitting signals between the brain and other parts of the body. They are specialized bundles of tissue composed of nerve cells, or neurons, along with supporting cells called glial cells. These neurons have extensions known as axons and dendrites that allow them to communicate with each other and with other cells in the body.
High Blood Glucose Levels (Hyperglycemia): Prolonged periods of elevated blood sugar levels in diabetes can damage the walls of the small blood vessels (microvascular damage) that supply oxygen and nutrients to nerves. This impaired blood flow can lead to nerve damage over time.
Advanced Glycation End Products (AGEs): When blood sugar levels are high, excess glucose can bind with proteins in the body, forming harmful molecules called advanced glycation end products. These AGEs can accumulate in nerve tissues and contribute to nerve damage and dysfunction.
👉foot neuropathy pain relief Chronic inflammation, a common feature of diabetes, can damage nerves directly or exacerbate existing nerve damage. Inflammatory processes can impair nerve function and contribute to neuropathic symptoms.
Oxidative Stress: Diabetes can lead to increased production of free radicals and decreased levels of antioxidants in the body, resulting in oxidative stress. This oxidative damage can affect nerve cells and contribute to the development and progression of neuropathy.
Insulin Resistance: Insulin resistance, a hallmark of type 2 diabetes, can contribute to nerve damage by impairing the ability of cells to take up glucose from the bloodstream. This can lead to higher levels of glucose in the blood and subsequent nerve damage.
Genetic Factors: Some individuals may have a genetic predisposition to developing diabetic neuropathy. Certain genetic factors may influence susceptibility to nerve damage in the presence of diabetes.
Duration of Diabetes: The longer someone has diabetes, especially if it is poorly controlled, the higher the risk of developing diabetic neuropathy. Chronic exposure to high blood sugar levels increases the likelihood of nerve damage.
Other Risk Factors: Several other factors can increase the risk of diabetic neuropathy, including obesity, high blood pressure, smoking, excessive alcohol consumption, and a sedentary lifestyle.
👉 Neuropathy, or nerve damage, can result in chronic pain, and tapentadol is an opioid analgesic that works by binding to receptors in the brain and spinal cord to alleviate pain.
What are the symptoms of neuropathic pain?
Neuropathic pain can stem from various conditions and factors that affect the nerves. Here’s a breakdown of some of the common causes:
Alcohol Use Disorder: Chronic alcohol abuse can lead to nerve damage, resulting in neuropathic pain.
Diabetes: High blood sugar levels associated with diabetes can cause nerve damage, particularly in the feet and hands, leading to diabetic neuropathy.
Facial Nerve Conditions: Conditions affecting the facial nerves, such as trigeminal neuralgia, can cause neuropathic pain in the face.
HIV/AIDS: The virus itself or medications used to treat HIV/AIDS can damage nerves, leading to neuropathic pain.
Central Nervous System Disorders: Conditions like stroke, Parkinson’s disease, and multiple sclerosis (MS) can affect the central nervous system and result in neuropathic pain.
Complex Regional Pain Syndrome: CRPS is a chronic pain condition that usually affects one limb following an injury or trauma.
Shingles: The varicella-zoster virus, which causes chickenpox, can reactivate later in life and cause shingles, resulting in neuropathic pain along affected nerves.
Other causes of neuropathic pain can include:
Chemotherapy Drugs: Certain chemotherapy drugs can cause nerve damage, leading to neuropathic pain.
Radiation Therapy: Radiation treatment for cancer can also damage nerves, causing neuropathic pain in the affected area.
Amputation: After an amputation, some individuals may experience phantom limb pain, where they feel pain in the missing limb.
Spinal Nerve Compression or Inflammation: Conditions such as herniated discs or spinal stenosis can compress or inflame spinal nerves, leading to neuropathic pain.
Trauma or Surgeries: Injuries or surgeries that result in nerve damage can cause chronic neuropathic pain.
Tumors: Tumors pressing on nerves can cause neuropathic pain in the affected area.
These are just some of the many potential causes of neuropathic pain, and treatment often involves addressing the underlying condition along with managing the pain symptoms.
Medication for Neuropathic Pain
Here are some medications commonly used to manage neuropathic pain:
- Opioid Analgesics: In cases of severe neuropathic pain that does not respond to other treatments, opioid medications may be prescribed for short-term use. Examples include Aspadol 200mg and oxycodone (OxyContin).
- Gabapentin (Neurontin): Gabapentin medication like Neurontin 100mg is an anticonvulsant medication that is often prescribed to treat neuropathic pain. It works by modulating the activity of certain neurotransmitters involved in pain signaling.
- Pregabalin (Lyrica): Pregabalin is another anticonvulsant medication such as Lyrica 150mg is similar to gabapentin and is used to treat neuropathic pain conditions such as diabetic neuropathy and postherpetic neuralgia.
The effectiveness of these medications can vary from person to person, and they may also be associated with side effects. Always consult with a healthcare professional for proper diagnosis and guidance on the most appropriate treatment for your neuropathic pain.
 English
English
 French
French  German
German