Sorry, nothing in cart.
Osteoarthritis Pain Cause, Symptoms, Risk, Diagnosis & Treatment
- By admin
- |
- General Blog
- |
What is Osteoarthritis?
Osteoarthritis is a degenerative joint disease in which the tissues of the joints regularly degenerate. It is the most widespread type of arthritis and affects older people more frequently.
Osteoarthritis patients frequently report joint pain and stiffness following periods of inactivity or rest.
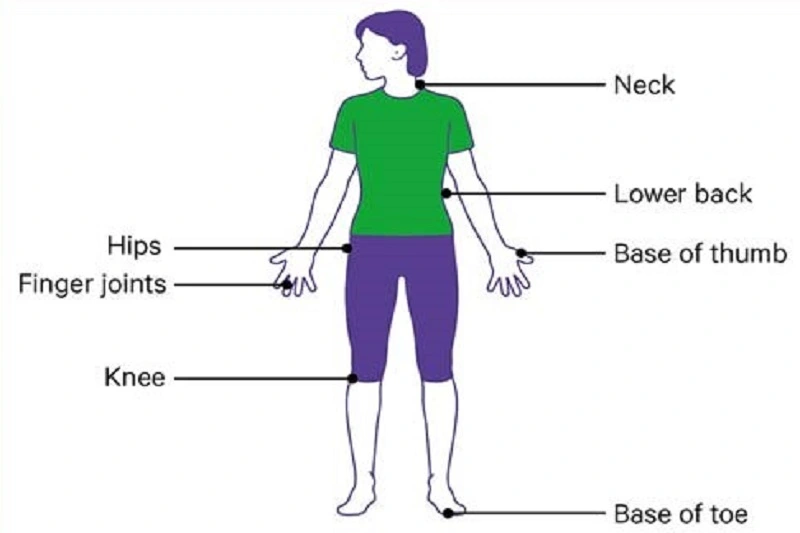
The following joints are the most typically affected:
- Hands (at the fingertips as well as the base and ends of the thumbs).
- Knees
- Hips
- Neck
- The lower back
Each person is affected differently by osteoarthritis. Some people have mild osteoarthritis, which does not affect their ability to go about their regular lives. It causes substantial pain and incapacity for others. Joint injury often develops over time, though it might worsen quickly in some persons.
What occurs and when you Get Osteoarthritis?
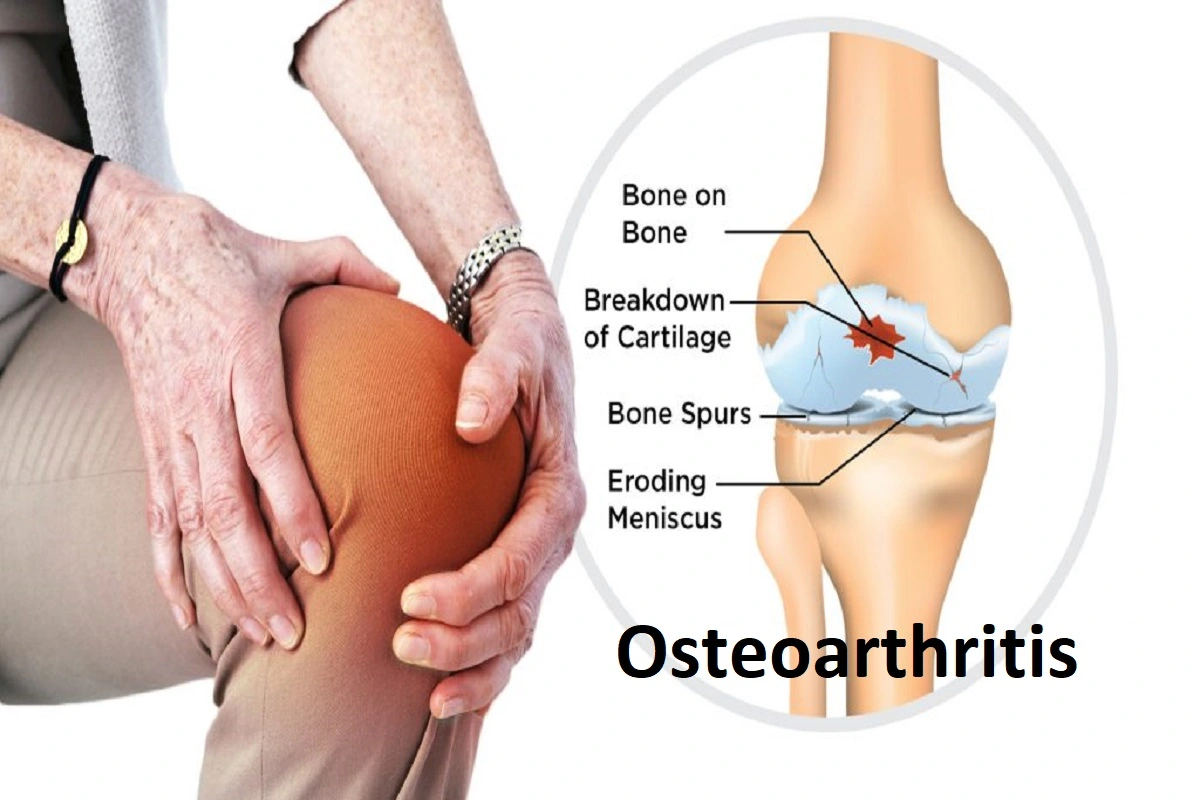
Researchers are unsure what causes or initiates the breakdown of the tissues in the joint. However, as osteoarthritis progresses, it may harm every area of the joint, including cartilage, the tissue that covers the ends of two bones that come together to form a joint.
- Ligaments and tendons.
- The synovium is the joint lining.
- Bone
- Knee meniscus tear.
Pain, swelling, and loss of joint motion develop as soft tissue injury in the joint proceeds. When you experience pain in your joints, you may be less active, which can lead to muscle weakness and put greater strain on the joint. Over time, the joint might lose its usual shape.
Small bone growths called osteophytes or bone spurs may also form on the joint’s borders. The bone’s form may also shift. Bone or cartilage particles can also break off and float inside the joint area. This creates even greater harm. Researchers are still looking into what causes pain in persons with osteoarthritis.
What Causes Osteoarthritis?
Osteoarthritis can affect anyone; however, it becomes more common as people age. Women are more sensitive than men to get osteoarthritis, particularly after the age of 50. It appears in many women after menopause.
Younger people can also get osteoarthritis, which is mainly caused by:
- Joint pain.
- The joint structure is abnormal.
- A genetic flaw in joint cartilage.
Other Causes of Osteoarthritis:
- Osteoarthritis occurs when the cartilage and other tissues within the joint affect or alter in structure.
- This is not due to normal wear and strain on the joints.
- Changes in the tissue, on the other hand, might cause disintegration, which normally occurs gradually over time.
- Certain variables may increase your chances of developing the condition, including:
- Aging.
- Obesity is being overweight.
- A history of joint damage or surgery.
- Overuse is caused by repetitive joint motions.
- Joints that do not properly develop.
- There is a family history of osteoarthritis.
Risk Factors of Osteoarthritis:

- Older age: is one factor that can increase your risk of osteoarthritis. Age increases one’s risk of developing osteoarthritis.
- Sex: It is unknown why women are more prone than males to acquire osteoarthritis.
- Obesity: Extra body weight leads to osteoarthritis in a variety of ways, and the more you weigh, the more likely you are to get it. Weight gain puts strain on weight-bearing joints like your hips and knees. Adipose tissue also produces substances that can cause significant inflammation in your joints.
- Injuries to the joints: Injuries, such as those experienced while playing sports or in an accident, might increase the risk of developing osteoarthritis. Even injuries that appear to have healed many years ago can raise your risk of osteoarthritis.
- The joint has been subjected to repeated stress: If your profession or an activity causes repetitive stress on a joint, that joint may develop osteoarthritis.
- Genetics: Some persons are predisposed to osteoarthritis.
- Deformities of the bones: Some people are born with faulty joints or cartilage.
- Certain metabolic conditions: Diabetes and hemochromatosis, a condition in which your body has an excessive amount of iron, are examples.
Osteoarthritis Symptoms

Osteoarthritis symptoms usually appear gradually and begin with one or a few joints. The following are some of the most common symptoms of osteoarthritis:
- Pain when use of the joint may go away with rest. In the later stages of the disease, some people may experience more pain at night. Pain can be localized or generalized.
- Joint stiffness that lasts less than 30 minutes, commonly in the morning or after a period of rest.
- Changes in the joints that may block joint movement.
- Swelling in and around the joint, particularly after extensive activity or use of that area.
- Changes in the joint’s ability to move.
- The sensation that a joint is loose or unstable.
Osteoarthritis symptoms can impact joints in a variety of ways. As an example:
- Hands: Finger joint enlargements and form alterations can occur over time.
- Knees: You may hear a grinding or scraping noise while walking or moving. Muscle and ligament weakening can cause the knee to buckle over time.
- Hips: You may experience pain and stiffness in the hip joint, as well as the groin, inner thigh, or buttocks. Pain that comes from hip arthritis can sometimes radiate (spread) to the knees. You may find that you can’t move your hip as far as you used to.
- Spine: You can get stiffness and soreness in your neck or lower back. As the spine changes, some patients acquire spinal stenosis, which can cause various symptoms.
Activities that you may manage become difficult to do when your symptoms grow, such as stepping up, getting on or off the toilet or in and out of a chair, grasping a pan, or walking across a parking lot.
Osteoarthritis pain and associated symptoms can cause fatigue, difficulty sleeping, and depression.
Diagnosis
The medical history, physical examination, and lab tests all contribute to the OA diagnosis.
Your primary care physician may be the first person you consult regarding joint pain. The doctor will go through your medical history, symptoms, how the pain affects your daily activities, medical concerns, and prescription use.
In addition, he or she will examine and move your joints and may order imaging. These tests aid in the diagnosis:
Aspiration shared. After the area has been numbed, a needle is introduced into the joint to extract fluid. To rule out other medical illnesses or kinds of arthritis, this test will look for infection or crystals in the fluid.
- X-ray: X-rays might reveal joint or bone injury or osteoarthritic changes.
- MRI: Magnetic resonance imaging (MRI) provides a more detailed image of cartilage and other joint components.
Treatment
There is no cure for OA, however, medication, assistive devices, and other non-drug therapy can help relieve pain. A damaged joint can be medically repaired or, as a last option, replaced with one made of metal, plastic, and ceramic composite.
Medications
Osteoarthritis pain and anti-inflammatory medications are available as follows:
Tapentadol (Opioid Analgesic):
Tapentadol (Opioids Analgesic) is a Strong pain medication prescribed when pain is uncontrolled. It is effective for Pain treatment in acute and chronic conditions.
NSAIDs are Nonsteroidal Anti-Inflammatory Medicines:
These are the most regularly used anti-inflammatory and pain medications. Celeheal 100 mg (Celecoxib) are example of OTC and prescription medication. The over-the-counter medications relieve pain but not inflammation.
Antidepressant and Anticonvulsants
- Antidepressant: Dulane 20 mg (Duloxetine)
- Seizure Medication (Anticonvulsants): Pregabalin (Lyrica)
Both are FDA-approved oral medications for the treatment of OA pain.
FAQS:
What does the pain of osteoarthritis feel like?
The joints in osteoarthritis may be achy and sensitive, but they may not appear swollen or heated (as joints in RA do). Greater edema may occur after physical exercise, and greater swelling may occur as the condition progresses.
Is the discomfort from osteoarthritis constant?
Osteoarthritis is a progressive degenerative disease that frequently causes chronic pain. Joint pain and stiffness can become so severe that ordinary tasks become challenging.
How long does a flare-up of osteoarthritis last?
A flare-up of symptoms is usually caused by an incident of inflammation within the joint. A flare-up is so expected to persist between 6 and 12 weeks.
When is the worst time of day for Joint Pain?
People with arthritis typically have more acute pain and stiffness first thing in the morning: “Joints associated with Joint Pain often stiffen up in the mornings and can make nights painful and restless.”
What is the most effective treatment for Joint Pain?
Lifestyle modifications, such as keeping a healthy weight and exercising regularly, are the primary treatments for osteoarthritis symptoms. Medication – to alleviate your discomfort. Supportive therapy – to assist in making daily chores simpler.
What causes Joint pain?
Extra body weight contributes to joint pain in a variety of ways, and the more you weigh, the greater your risk. Weight gain puts strain on weight-bearing joints like your hips and knees. Adipose tissue also produces chemicals that can cause significant inflammation in and around your joints. Injuries to the joints.
 English
English
 French
French  German
German