Sorry, nothing in cart.
PAH – Types, Causes
- By admin
- |
- General Blog
- |
Pulmonary arterial hypertension (PAH) is a type of pulmonary hypertension (high blood pressure in the lungs).
The pulmonary arteries harden and become dysfunctional in PAH. As the condition advances, they may thicken or narrow.
The heart must work harder to push blood through the narrowed arteries. This causes an increase in pulmonary blood pressure.
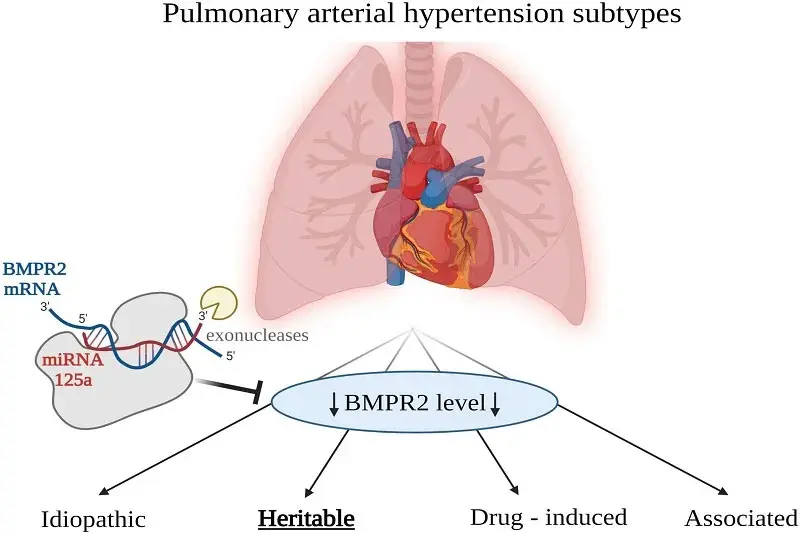
Types of Pulmonary Arterial Hypertension
The most prevalent types of pulmonary arterial hypertension (PAH) are as follows:
Idiopathic: Pulmonary hypertension, commonly known as idiopathic pulmonary artery hypertension (IPAH), is a progressive condition affecting the precapillary pulmonary vasculature with no recognized cause.
Heritable: Heritable pulmonary arterial hypertension (HPAH) occurs as a result of PAH predisposing gene mutations or in a familial environment. HPAH is characterized by increased pulmonary arterial resistance, which results in right heart failure.
Drug and toxin-induced: D-PAH is a type of World Health Organization Group 1 pulmonary hypertension (PH) characterized by significant small vessel loss and obstructive maculopathy, which leads to right heart failure and death.
Measuring blood pressure
Most people have had their blood pressure checked with a blood pressure cuff. This cuff monitors the pressure in your heart’s left side in millimeters of mercury (or mm Hg). Your blood pressure reading is divided into two parts:
Systolic: The greater the number, the greater the pressure as your heart beats.
Diastolic: The smaller value represents the pressure while your heart is at rest between beats.
A normal blood pressure value is greater than 120 (systolic) and less than 80 (diastolic).
The pressure in the right side of your heart is measured by the blood veins in your lungs, not your heart. Your pulmonary artery pressure (PAP) is measured here. At repose, normal PAP ranges from 8 to 20 mm Hg. This metric is deemed high if it is greater than 25 mm Hg at rest or 30 mm Hg during physical activity.
How does PAH affect your heart and the arteries of your lungs?
PAH may make blood flow through your lungs difficult. As a result, your heart has to work more than usual to deliver blood into the arteries of your lungs. This can cause the muscles of your heart to thicken over time. This can make your heart’s job of pumping blood to your body more challenging.
Symptoms of Pulmonary Arterial Hypertension
- Breathing difficulties during everyday activity
- Fatigue
- Chest ache
- The heartbeat is racing.
- Upper right side of the abdominal pain
- Appetite suppression
- Wheezing and coughing
- Lightheadedness, especially during strenuous exercise
- Fainting
- Ankle and leg swelling
Causes
- Scleroderma and rheumatoid arthritis are examples of autoimmune illnesses that cause lung damage.
- Heart defects at birth
- Pulmonary embolism is the formation of blood clots in the lungs.
- Heart failure (of the left ventricle)
- Valve disease of the heart
- Infection with HIV
- Long-term (chronic) low oxygen levels in the blood
- COPD, pulmonary fibrosis, and other severe lung diseases
- A persistent pulmonary disease
- Medicines (such as certain diet pills)
- Obstructive sleep apnea (OSA)
How Is Pulmonary Arterial Hypertension Detected?
Because the symptoms are similar to those of other prevalent lung disorders, PAH can be difficult to diagnose. Diagnosis is the process of excluding other disorders. You will need to conduct various tests with the help of lung and heart specialists (pulmonologist and cardiologist), such as:
Test of the blood: HIV tests, thyroid tests, autoimmune disease panels (including systemic lupus erythematosus, scleroderma, and rheumatoid arthritis), liver tests, and blood chemistry tests are all available.
Electrocardiogram: Displays the electrical activity of the heart and may aid in the detection of problems. Doctors may also be able to detect evidence of right-sided heart strain.
Lung function (breathing) tests: Checks for disorders such as asthma or COPD.
6-Minute Walk test: Measures how far you can walk objectively and whether your oxygen levels decline when you are physically active.
Echocardiogram: Ultrasound of the heart to determine the size and condition of the chambers. It can also be used to calculate pulmonary artery blood pressure.
Catheterization of the Right Heart: This test is intrusive, it is normally conducted only when other tests have failed to yield a definitive diagnosis. A catheter (small tube) is inserted into a major vein in the neck, arm, or groin and threaded through the right side of the heart and into the pulmonary artery. This allows for the measurement of pulmonary blood pressure.
Treatment Methods
Although most kinds of PH have no known cure, there are medications available to help treat PAH. These medications are based on naturally occurring substances in your body that may be out of balance.
Endothelin Receptor Antagonists (ERAs):
These are drugs that are taken orally (by mouth). Endothelin overproduction causes blood vessels to constrict and tighten. This can result in excessive blood pressure in the lungs.
Phosphodiesterase Inhibitors (PDE-5):
These are drugs that are taken orally (by mouth). PDE-5 functions similarly to nitric oxide.
Nitric oxide aids in the relaxation of blood vessels. Low amounts of this can cause pulmonary hypertension.
Medications that increase nitric oxide production in the body to assist relax blood arteries include:
Prostacyclin:
These medications are classified as:
Inhaled (breathed in) into the body via a catheter (tube) orally (by mouth). Oral prostacyclin are newer PAH medications.
Keeps arteries open so blood can circulate freely. Too little of this in your body may raise blood pressure in your lungs.
Oxygen:
This can aid in the relaxation of blood vessels in the lungs.
Anticoagulants:
They are referred to as “blood thinners.” These are occasionally used to treat blood clots in the lungs.
Diuretics:
Also known as “water pills.” These are used to reduce edema in the belly, legs, or foot.
Prevent difficulties throughout your life.
Your doctor may advise you to take the following to help prevent some of the problems of pulmonary hypertension.
- If your pulmonary hypertension is caused by heart failure or high blood pressure, make heart-healthy lifestyle adjustments such as heart-healthy nutrition.
- Participate in frequent physical activity. Consult your doctor before beginning any fitness program to determine the right level of physical exercise for you.
- Avoid high altitudes if possible, and consult your doctor about any plans for air travel or visits to high-altitude regions.
- If you intend to become pregnant, consult your doctor because there is an elevated risk of pregnancy difficulties.
- Treat additional medical issues such as COPD, heart disease, and Narcolepsy.
FAQs
Q1) what is the life expectancy of someone with pulmonary arterial hypertension?
Ans: The type of PH you have and the source of your PH will determine your life expectancy. People with group 1 PAH have a median survival time of more than 5 years after diagnosis.
Q2) what is the main cause of pulmonary hypertension?
Ans: High blood pressure in the lungs arteries due to some types of congenital heart disease, connective tissue disease, coronary artery disease, high blood pressure, liver disease (cirrhosis), blood clots to the lungs, and chronic lung diseases like emphysema are some of the most common underlying causes of pulmonary hypertension.
Q3) what are the 4 stages of pulmonary hypertension?
Ans: Stages of pulmonary arterial hypertension
Class 1: Your physical activity is not restricted.
Class 2: The ailment limits your physical activity slightly.
Class 3: The condition severely restricts your physical activity.
Class 4: You are unable to engage in any physical activity without experiencing symptoms.
Q4) Can pulmonary hypertension go away?
Ans: Although pulmonary hypertension cannot be cured, medication can alleviate symptoms and assist you in managing your condition. Pulmonary hypertension typically worsens over time.
Q5) what should I avoid if I have Pulmonary arterial hypertension?
Ans: If you have PAH, you should avoid foods that are heavy in salt or sodium, such as:
- Food in cans.
- Foods that have been processed.
- Meats from a deli.
- Various seasonings.
- Dinners from the freezer.
- Fermented foods.
Q6) what test confirms Pulmonary arterial hypertension?
Ans: The most popular tests for measuring pulmonary artery pressure are cardiac catheterization and echocardiography. Normal pulmonary artery pressure ranges between 11 and 20 millimeters of mercury (mm Hg). You may have pulmonary hypertension if your blood pressure is excessively high.
Q7) what is the difference between pulmonary hypertension and pulmonary arterial hypertension?
Ans: Pulmonary arterial hypertension (PAH) is a subtype of pulmonary hypertension, which is defined as excessive blood pressure in the lungs. This elevated pressure in the vasculature in PAH is produced by a number of obstructions in the tiny arteries of the lung.
Q8) at what age do you get Pulmonary arterial hypertension?
Ans: Women are more affected than males by PAH.
According to the PH Association, idiopathic and heritable forms of PAH are at least twice as frequent in women as in males. In fact, PAH is most commonly diagnosed in women aged 30 to 60.
Q9) is drinking water good for Pulmonary arterial hypertension?
Ans: When you consume an excessive amount of fluid, your heart needs to work significantly harder to circulate the extra fluid throughout your body. This can aggravate your heart issues. Limiting fluid intake is critical for avoiding ER visits and hospital admissions.
Q10) what are the symptoms of end stage Pulmonary arterial hypertension?
Ans: End-Stage Pulmonary arterial hypertension Monitoring
As PH advances, a person’s symptoms, such as shortness of breath, fluid retention, and chest pain, may increase. Hypoxia (low blood oxygen) can result from impaired lung function, causing dizziness, light-headedness, and syncope (fainting).
 English
English
 French
French  German
German