Sorry, nothing in cart.
GLP-1 receptor agonists for Type 2 Diabetes
- By admin
- |
- General Blog
- |
GLP-1 receptor agonists have transformed the management of type 2 diabetes (T2DM) and obesity. These drugs have been demonstrated to improve glycemic management, reduce body weight, and reduce the risk of cardiovascular events. This blog will investigate glucagon-like peptide-1 agonists, including their mechanism of action, advantages, and potential adverse effects.
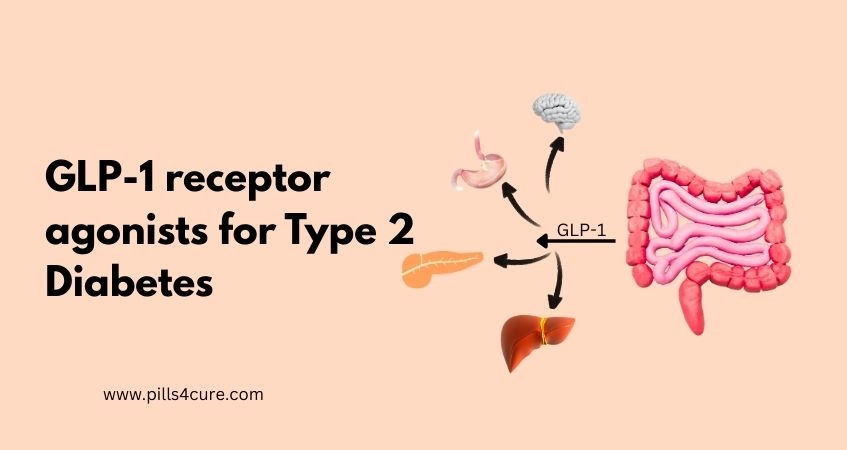
What is GLP-1
GLP-1 (Glucagon-Like Peptide-1) is a natural hormone made in your intestines. It is released after you eat, and its main job is to help your body manage blood sugar and control appetite.
Think of GLP-1 as a helper hormone that tells your body:
- “Make more insulin now — food has arrived!”
- “Stop releasing glucagon — we don’t need extra sugar in the blood.”
- “Slow down stomach emptying — make the person feel full.”
Because of these effects, GLP-1 helps keep blood sugar levels stable and also reduces hunger.
GLP-1 Receptor (GLP1R): Structure and Function
GLP-1R stands for Glucagon-like Peptide-1 Receptor. It is also known as a G protein-coupled receptor (GPCR). You can find this receptor on the beta cells of the pancreas and on neurons in the brain. It actively responds to the GLP-1 hormone and triggers several metabolic actions. It helps regulate blood sugar levels by improving insulin activity. The GLP1R gene on chromosome 6 produces this receptor. GLP-1R belongs to the glucagon receptor family and functions as a G-protein–coupled receptor.
GLP1R has two parts: an extracellular domain (ECD) that binds the C-terminal helix of GLP-1 and a transmembrane domain (TMD) that binds the N-terminal region of GLP-1. A centre of polar residues in the TMD domain controls the biased signalling of the receptor. The transmembrane helix boundaries and the outside of cells cause biased agonism.
How Do GLP-1 Receptor Agonists Work?
GLP-1 Receptor Agonists (RA), sometimes known as Glucagon-Like Peptide-1 receptor agonists, imitate the effects of natural GLP-1. They connect to GLP-1 receptors on pancreatic beta cells, increasing insulin release while decreasing glucagon release. This leads to better glycemic control, a lower appetite, and higher sensations of fullness.
Molecular mechanisms:
Glucagon-like peptide-1 receptor agonists interact with pancreatic beta cells’ GLP-1 receptors, boosting insulin release while blocking glucagon release. This causes a drop in blood glucose levels. Furthermore, GLP-1 receptor agonists delay stomach emptying, lowering peak blood glucose levels after meals.
At the molecular level, GLP-1 receptor agonists activate the glucagon-like peptide-1, initiating a signalling cascade that:
Increases insulin secretion: glucagon-like peptide-1 receptor agonists promote insulin release from pancreatic beta cells, lowering blood glucose levels.
Inhibits glucagon secretion: GLP-1 receptor agonists reduce glucagon release, which boosts blood glucose levels.
Slows gastric emptying: GLP-1 receptor agonists slow gastric emptying, lowering peak blood glucose levels after meals.
Increases satiety: GLP-1 receptor agonists increase satiety mainly by acting on appetite-regulating centers in the brain and by slowing gastric emptying.
Differences from Other Diabetes Medications:
GLP-1 receptor agonists differ from other diabetic treatments in the following ways:
Mechanism of action: GLP-1 receptors mimic the action of natural GLP-1, whereas other diabetic medicines, such as sulfonylureas and meglitinides, promote insulin release via distinct processes.
Glucose-dependent insulin secretion: GLP-1 receptor increases insulin production only when blood glucose levels rise, lowering the risk of hypoglycemia. In contrast, sulfonylureas and meglitinides can increase insulin secretion even when blood glucose levels are low, increasing the risk of hypoglycemia.
Weight reduction: GLP-1 receptors have been associated with significant weight loss, whereas many other diabetes treatments can lead to weight gain.
Cardiovascular advantages: GLP-1 receptors have been demonstrated to lower the risk of major adverse cardiovascular events (MACE), such as heart attacks and strokes, although the cardiovascular benefits of other diabetes drugs are less certain.
Advantages of GLP-1 Receptor agonists
There are several benefits to GLP-1 receptor agonists, including:
Improved glycemic control:
- Glucagon-like peptide-1 receptor agonists have been demonstrated to lower HbA1c levels, which are an indicator of average blood glucose management. As mentioned, the reduction of 1.04% is consistent with findings from various studies, though the exact reduction can vary depending on the specific drug and population studied.
Weight reduction:
- GLP-1 receptor agonists have been proven to aid in weight loss, particularly in obese patients. After 20 weeks, weight loss was 5.5 kg (12.1 lbs), consistent with clinical findings. Weight loss can vary by individual and study duration.
Reduced cardiovascular risk:
- Studies have demonstrated that GLP-1 receptor agonists lower the risk of cardiovascular events like heart attacks and strokes. In the SUSTAIN-6 study, semaglutide reduced MACE by 26% compared to placebo. GLP-1 receptor agonists help the heart, according to these data.
Improved blood pressure control:
- GLP-1 receptor agonists have been found to lower blood pressure in hypertensive people. According to published data, liraglutide lowers systolic blood pressure by 2.6 mmHg, though results may vary.
Improved lipid profiles:
- Studies have demonstrated that GLP-1 receptor agonists enhance lipid profiles, lowering the risk of cardiovascular disease. These percentages (19.6% reduction in triglycerides and 10.3% increase in HDL cholesterol) are consistent with clinical trials. However, they may vary by patient demographic and treatment.
Examples of Glucagon-Like Peptide-1 receptor Agonists:
There are several GLP-1 receptor agonists for Type 2 Diabetes on the market now, including:
Ozempic (Semaglutide): Ozempic (Semaglutide) is a once-weekly injectable drug that enhances glycemic management and aids in weight loss. Dosage are: Ozempic 0.25mg, Ozempic 0.5mg, Ozempic 1mg
Trulicity (dulaglutide): Trulicity is a once-weekly injectable drug found to enhance glycemic management while lowering cardiovascular risk.
Rybelsus (Semaglutide tablets): This oral drug has been found to enhance glycemic management and increase weight loss. Dosage are: Rybelsus 3mg, Rybelsus 7mg, Rybelsus 14mg
Possible Side Effects of GLP-1 Receptor Agonists
GLP-1 receptor agonists are generally well tolerated. However, they can induce some side effects, including:
- Nausea and Vomiting: GLP-1 receptor agonists can produce nausea and vomiting, especially when first used.
- Diarrhoea: GLP-1 receptor agonists can cause diarrhoea, especially in people with irritable bowel syndrome.
- Injection site reactions: GLP-1 receptor agonists may produce injection site responses such as redness, oedema, and itching.
- Hypoglycemia: GLP-1 receptor agonists have a low risk of hypoglycemia when used alone, but the risk increases when combined with insulin or sulfonylureas.
- Pancreatitis: GLP-1 receptor agonists have been linked to an increased risk of pancreatitis, an uncommon but severe side effect.
Study Other Side Effects
Contraindications and precautions
Glucagon-like peptide-1 receptor agonists are contraindicated in those with:
- Type 1 diabetes: Glucagon-like peptide-1 has not been licensed for use in people with type 1 diabetes.
- Severe gastrointestinal disease: Glucagon-like peptide-1 may worsen gastrointestinal disorders like gastroparesis.
- Pregnancy and breastfeeding: Glucagon-like peptide-1 is not indicated for use while pregnant or nursing.
- Medullary Thyroid Carcinoma (MTC) / MEN2: GLP-1 receptor agonists are contraindicated in patients with a personal or family history of MTC or MEN2 syndrome.
Conclusion
Glucagon-like peptide-1 receptor agonists have transformed the management of Type 2 Diabetes and obesity. These drugs have been demonstrated to enhance blood sugar control, encourage weight loss, and lower cardiovascular risk. They understood how GLP-1 receptor agonists function and their benefits, allowing you to make more informed health decisions. Remember to consult your doctor about GLP-1 receptor agonists and take charge of your health today!
Frequently Asked Questions:
Q1) What’s the distinction between GLP-1 receptor agonists and insulin?
Ans: Glucagon-like peptide-1 receptor agonists imitate the activity of natural GLP-1, whereas insulin is a hormone that directly reduces blood sugar levels.
Q2) Can I take GLP-1 receptor agonists alongside other diabetic medications?
Ans: Yes, Glucagon-like peptide-1 receptor agonists can be administered alongside other diabetes drugs, such as metformin, sulfonylureas, and insulin. However, consulting your healthcare professional about potential interactions and changes to your treatment plan is critical.
Q3) Are GLP-1 receptor agonists suitable for long-term use?
Ans: GLP-1 receptor agonists have been proven safe for extended use, with some trials demonstrating efficacy and safety for up to two years.
Q4) Are GLP-1 receptor agonists available in oral or injectable form?
Ans: GLP-1 agonists are available in both oral and injectable versions. Typically, patients administer the injectable formulations once a week while they take the oral forms daily. Patient choices and needs determine whether to use oral or injectable forms.
Q5) Can persons without diabetes use GLP-1 receptor agonists to lose weight?
Ans: While Glucagon-like peptide-1 receptors were initially authorized for type 2 diabetes, they have also been found to benefit weight loss in those without diabetes. However, the off-label use of GLP-1 receptor agonists for weight loss in non-diabetics warrants consultation with a medical expert.
Q6) Are GLP-1 agonists safe for people with a history of pancreatitis?
Ans: GLP-1 receptor agonists have been linked to an increased risk of pancreatitis; however, the absolute risk remains modest. People with a history of pancreatitis, on the other hand, should consult their doctor before beginning treatment to evaluate the risks and advantages.
Q7) Can patients with kidney disease use GLP-1 agonists ?
Ans: People with renal disease can use GLP-1 receptor agonists , but the severity of their kidney impairment may require a change in dosage. Before beginning therapy, consult a healthcare practitioner about the risks and benefits.
Q8) How long does it take to see the results of the Glucagon-like peptide-1 receptor?
Ans: GLP-1 receptor agonists can produce effects such as improved glycemic control and weight loss within a few weeks to a few months of starting medication. However, realizing the full advantages may take many months or a year.
Q9) Is it possible to treat thyroid cancer with GLP-1 receptor agonists?
Ans: Ans: No, GLP-1 receptor agonists do not treat thyroid cancer. They are strictly contraindicated (must be avoided) in patients with a history of Medullary Thyroid Carcinoma (MTC) or MEN2 syndrome due to a potential risk of promoting tumor growth. While 2025 data suggests no increased risk for the general population, patients with thyroid history must consult an endocrinologist before use.